Dermatologist Offers Best Practices for Social Media Posts Dermatologist Offers Best Practices for Social Media Posts
August 20, 2024Neoadjuvant Immunotherapy Shows Promise for High-Risk HCC Neoadjuvant Immunotherapy Shows Promise for High-Risk HCC
August 20, 2024Personalized, adaptive deep brain stimulation (DBS) can enhance the control of motor symptoms of Parkinson’s disease (PD) compared with standard DBS, new research suggests.
In a blinded randomized crossover pilot trial involving four patients, adaptive DBS reduced the time spent with motor symptoms by half and improved patients’ quality of life compared with standard DBS.
“This is the future of deep brain stimulation for Parkinson’s disease,” study investigator Philip Starr, MD, PhD, professor of neurological surgery and co-director of the University of California San Francisco (UCSF) Movement Disorders and Neuromodulation Center, said in a statement.
“Adaptive DBS represents a major breakthrough in managing the symptom fluctuations in Parkinson’s disease by tailoring stimulation in real time to patients’ specific needs,” Carina Oehrn, MD, PhD, research fellow in the Starr Lab at UCSF, told Medscape Medical News.
The study was published online on August 19 in Nature Medicine.
A New Era of DBS?
DBS is a standard therapy for advanced PD. Standard DBS provides continuous, fixed stimulation that is unresponsive to patient activities or variations in severity of symptoms during daily life.
“While this approach effectively reduces motor symptoms for many patients, it does not account for the dynamic nature of PD symptoms, which can fluctuate throughout the day — for example, in response to medication. As a result, patients can experience breakthrough PD symptoms at times when they theoretically require more stimulation and stimulation-induced side effects when they would need less,” Oehrn told Medscape Medical News.
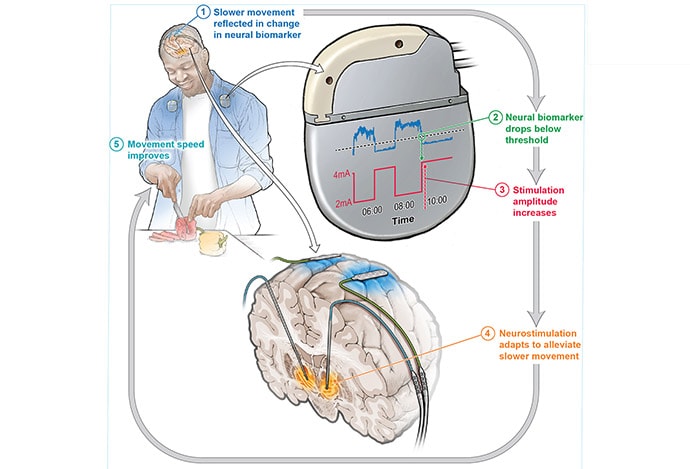
Adaptive DBS adjusts the intensity of stimulation based on the patient’s need — increasing stimulation when PD symptoms break through and decreasing stimulation at other times to prevent potential side effects caused by stimulation, she explained.
For their pilot trial, the UCSF team recruited four men with PD from a population undergoing DBS implantation for motor fluctuations, with each patient receiving adaptive DBS and continuous DBS.
Using a data-driven approach, they identified brain activity signals in the subthalamic nucleus and motor cortex that were reliable biomarkers of medication fluctuations and associated PD motor symptoms and used it to personalize the DBS parameters.
They found that adaptive DBS reduced the duration of motor symptoms by 50% compared with clinically optimized standard DBS. Objective measurements obtained by wearable devices confirmed the superiority of adaptive vs standard DBS. Three of the four patients also reported improved quality of life with adaptive DBS.
Ready for Prime Time?
Adaptive DBS shows “great promise” but widespread implementation will likely take a few more years, Oehrn told Medscape Medical News.
She noted that a highly specialized and interdisciplinary team was required to create a reliable, individualized algorithm for each patient. “The next step is to automate this process. This automation is crucial for making adaptive DBS more accessible and scalable for widespread clinical use,” Oehrn said.
A broader adoption of adaptive DBS will also require further clinical trials with a larger cohort to confirm the findings. Additionally, clinician training will be essential, as adaptive DBS involves complex, specialized decision-making, Oehrn cautioned.
“Once these challenges are addressed, adaptive DBS could become a very promising alternative to standard DBS for PD patients with motor fluctuations,” Oehrn said.
“In the meantime, one could envision establishing adaptive DBS clinics within highly specialized core research centers, featuring interdisciplinary collaborations with teams experienced in this method,” Oehrn added.
‘Remarkable’ Results
Reached for comment, Megan Frankowski, PhD, program director, Division of Translational Research, National Institute of Neurological Disorders and Stroke (NINDS), called these early results “exciting” and said adaptive DBS could be a “game changer” for patients with PD.
With standard DBS for PD, many patients have “lingering symptoms, and finding the right stimulation parameters can be arduous. Having an adaptive DBS system that could be modified based on how a patient is doing could really change the field,” Frankowski explained.
“The benefit of adaptive DBS is that it changes based on what symptoms are present. It self-modulates stimulation, so you only get it when you need it,” she noted.
With publication of the Nature Medicine paper, “it’s really the first time we’ve actually seen an adaptive DBS algorithm for Parkinson’s kind of in the wild working at home, and the results are remarkable.”
“Given the small sample size, the next step would be to refine the algorithms and the system and do a larger study with more patients to see how it plays out,” Frankowski said.
Support for this research was provided by NINDS grants, the Thieman Foundation, and TUYF Charitable Trust Fund. Starr received support from Medtronic and Boston Scientific for fellowship education. Oehrn reported no relevant disclosures. Frankowski manages the NINDS grants that funded the study.
